Back to accreditation.
Training in thoracic ultrasound is mandatory for Respiratory Medicine trainees prior to completion of CCT (and preferably prior to ST5). Until now the JRCPTB Respiratory Medicine Curriculum has mandated this is via completion of the Royal College of Radiologists Focused and Level 1 Thoracic Ultrasound pathway.
Respiratory trainees have struggled to complete this due to the requirement to attend ‘at least one session per week over a period of no less than 3 months, with approximately five scans per session performed by the trainee’.
The pleural community have called for a recent change in curriculum and the British Thoracic Society have created a comprehensive training pathway for thoracic ultrasound that was published in 2020. This pathway provides guidance for all stages of ultrasound training – from novice to expert – and redirects the training responsibility from Radiologists to specialist Respiratory Physicians.
This document also recognises that other specialties – such as Intensive Care and Acute Medicine – are gaining competence in thoracic ultrasound and that trainees may be exposed to a greater degree out of hours.
A link to the document is here.
Outline
The first thing to note is that this pathway is complex and comprehensive. The document is worth reading several times.
The curriculum provides guidance for 4 operator pathways and requirements for progressing to each stage. These include:
- Emergency
- Primary
- Advanced
- Expert
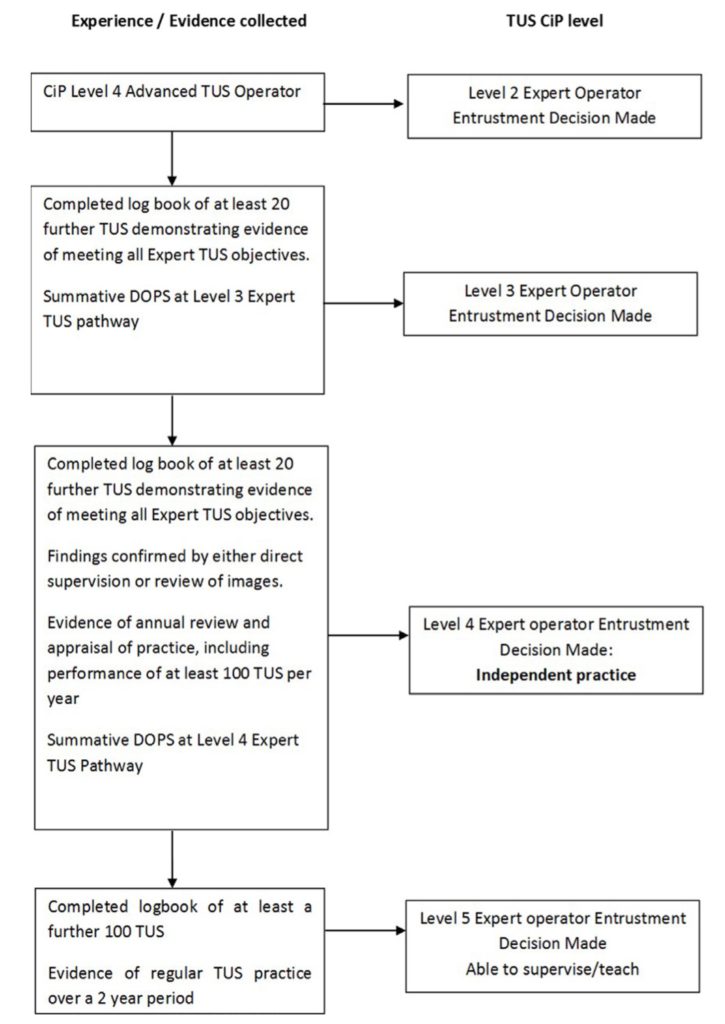
Each operator pathway is then separated into capabilities in practice (CiP) levels:
- Level 1 – entrusted to observe only with no provision of clinical care.
- Level 2 – entrusted to act with direct supervision within the room.
- Level 3 – entrusted to act with indirect supervision – supervisor may not be present in the hospital but contactable via electronic means and able to attend the bedside.
- Level 4 – entrusted to act unsupervised.
- Level 5 – able to supervise and train others.
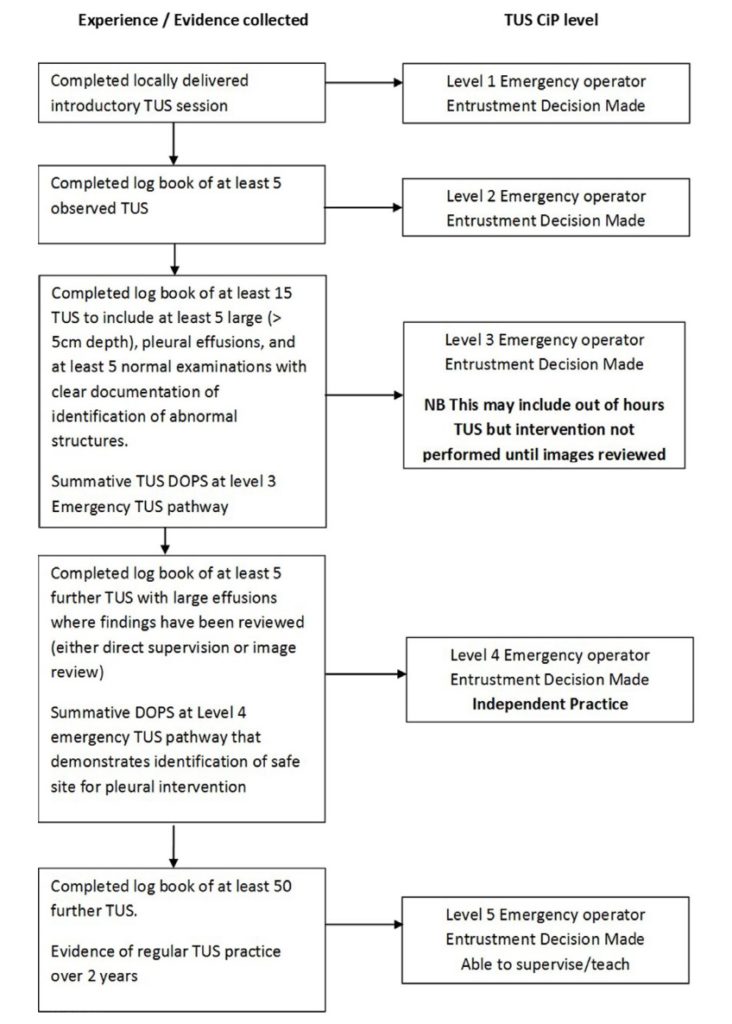
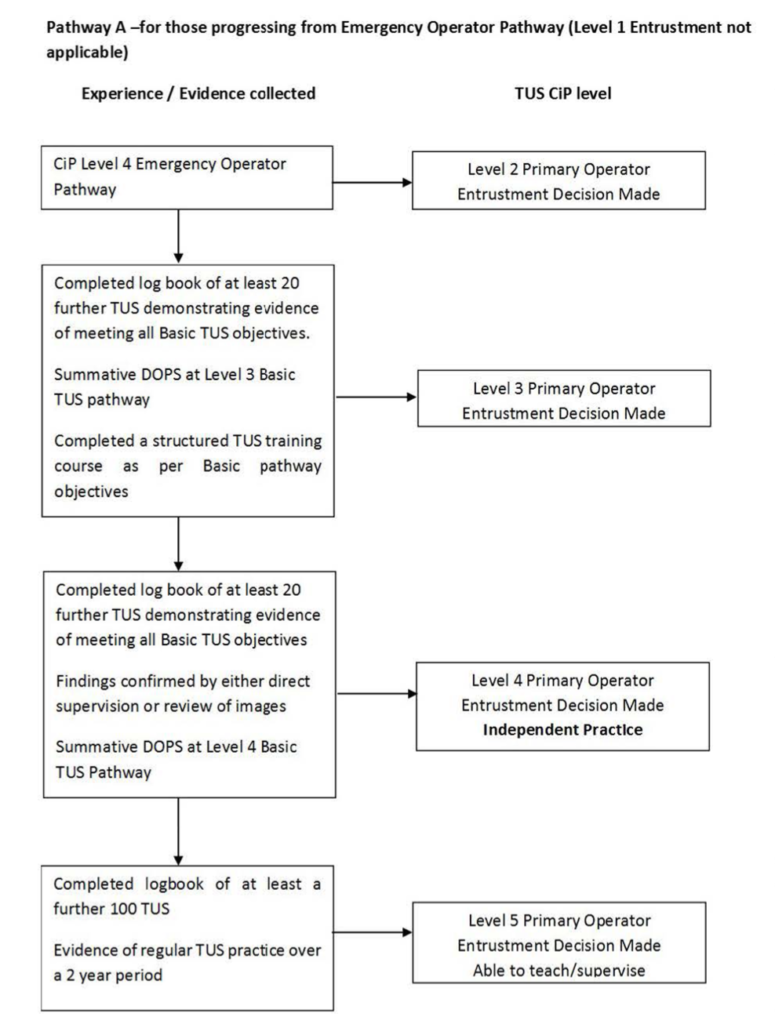
There are numeric and assessment requirements for each operator pathway and level within the pathway.
These steps are not necessarily linear and once level 4 is achieved in one operator pathway, scans may be used to progress within the next pathway.
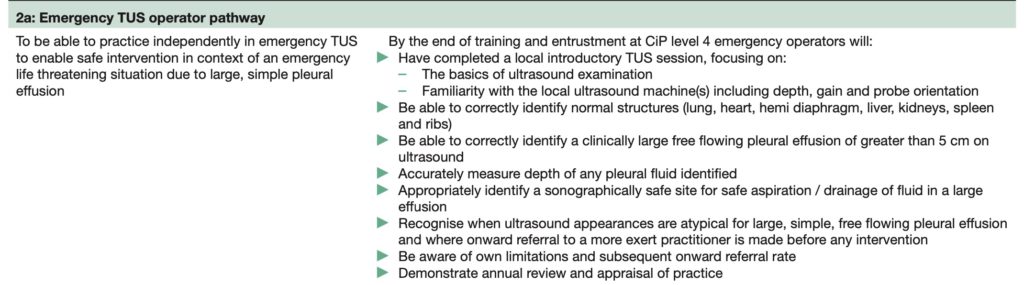
Emergency Operator
The aim of this operator pathway is to ensure there is a clinician out of hours capable of identifying a significant sized pleural effusion – measuring 5cm in size.
The key elements to this level is to be able to distinguish between different anatomical structures and recognise limitations and boundaries of their practice.
Curriculum:
Pathway:
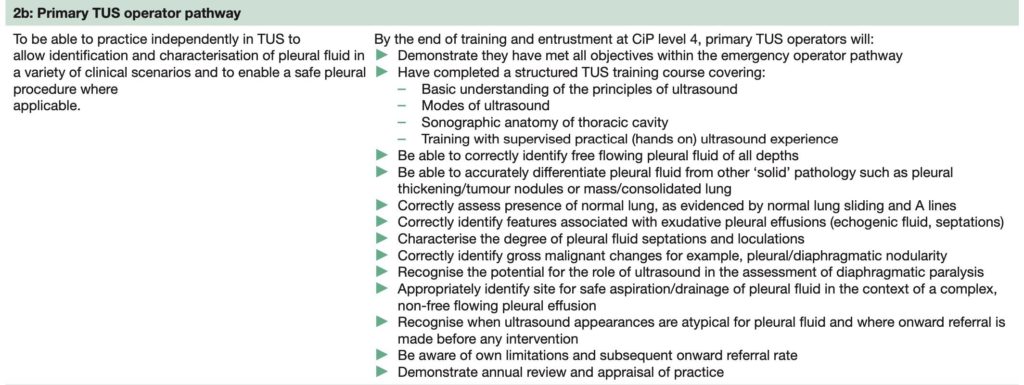
Primary Operator
Primary operator is now the equivalent to Level 1 RCR Thoracic US. It is the expected level that Respiratory Trainees should achieve by ST5 level and aims at identifying commonly encountered pathologies including:
- Smaller effusions
- Complex effusions
- Consolidated lung
- Pleural thickening
The trainee will be required to attend a dedicated and accredited course for Primary Thoracic US.
The aim of this pathway now is to make this level more achievable for Respiratory Trainees and integrate it into departmental teaching.
Curriculum:
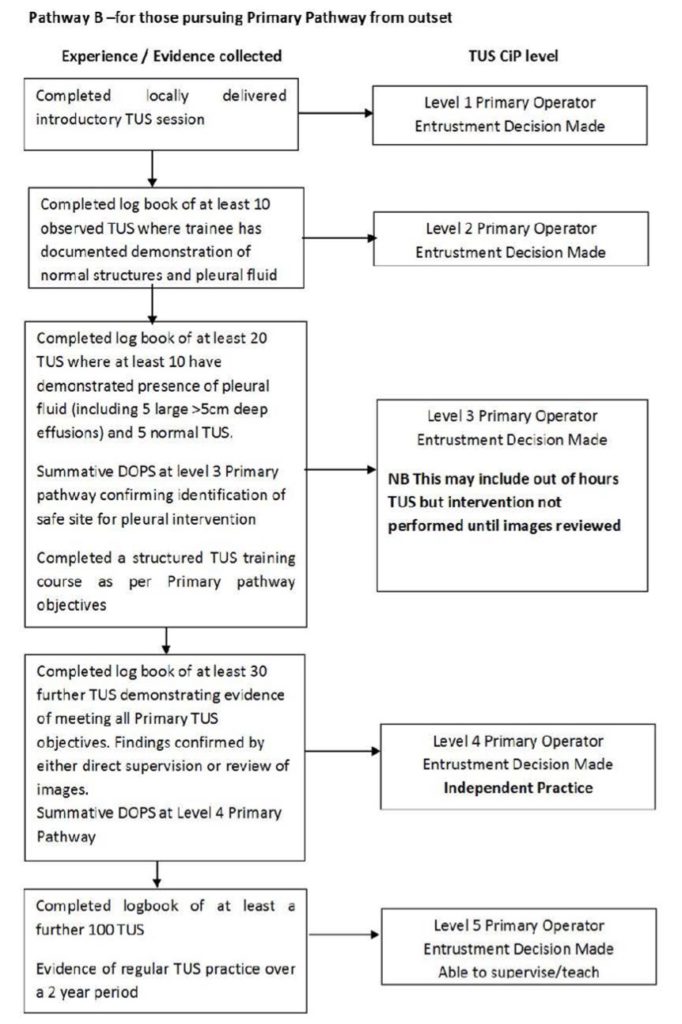
The BTS provide two separate training pathway guides for either:
- Trainees progressing from Emergency Operator level.
- Trainees seeking Primary Operator accreditation without prior experience.
Pathway progression from Emergency Operator:
Standalone pathway for Novices:
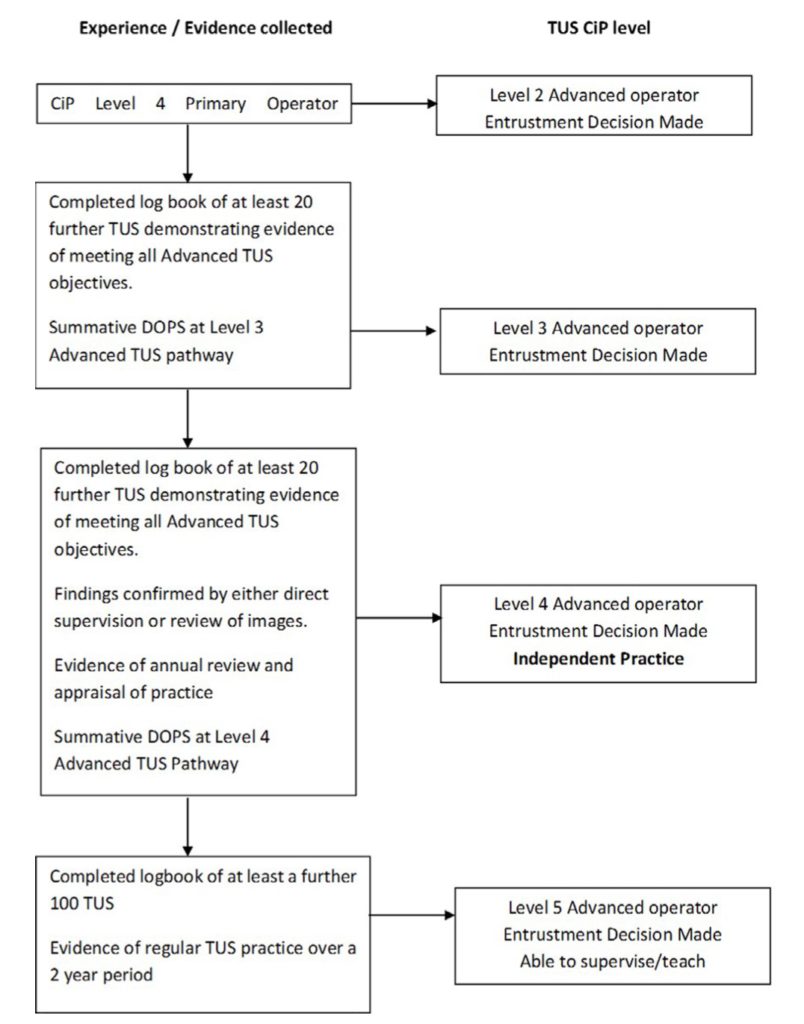
Advanced Operator
Advanced level is aimed at clinicians with regular pleural practice or a dedicated service.
They should have a minimum of 2 years at Primary level with evidence of ongoing practice in the field. It is aimed at the identification of more complex pathology including:
- Pneumothorax identification
- Diaphragmatic paralysis
- Artefact interpretation including B lines
- Ultrasound guided procedures including drains and thoracoscopy
It is not clear how this level will integrate with clinicians of other specialties who are already regularly performing thoracic ultrasound to identify more complex pathology.
Curriculum:
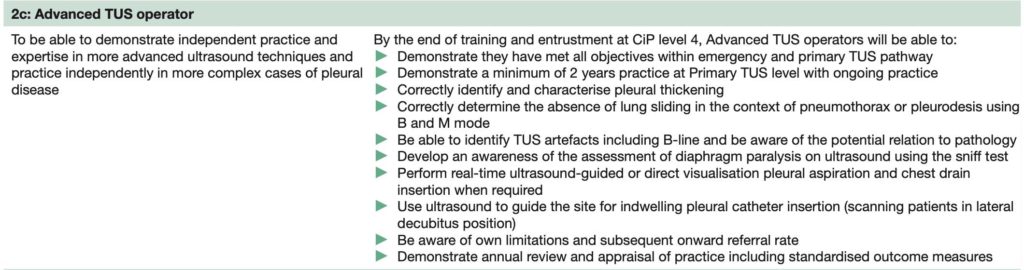
Pathway:
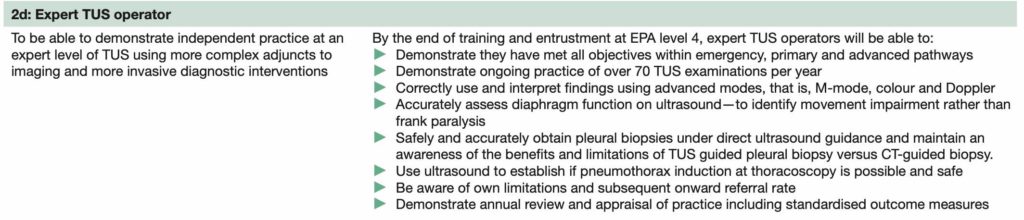
Expert Operator
Expert operators are expected to be using advanced ultrasound modes (M mode and colour doppler) and likely to be a pleural specialist. Expected common practice would involve:
- Assess diaphragmatic function, movement and thickening during respiration.
- Greater proficiency in US guided procedure.
- Pleural and lung biopsy – including pneumothorax induction for medical thoracoscopy.
It is appreciated that there will be existing practitioners who will not not be expected to gain formal sign off but must establish their level of expertise with a regional mentor.
Curriculum:
Pathway:
Maintenance of Competency
Ongoing practice is required for all disciplines to maintain competency. Local mentors may request supporting evidence (e.g. DOPS) if there is concern over capability.
Expected number of scans for maintenance of competency:
- Emergency operator – 5 scans per year.
- Primary operator – 20 scans per year.
- Advanced operator – 30 scans per year.
- Expert operator – 70 scans per year.
The new BTS guidance is a lengthy and complex guidance but aims to encompass all levels of ultrasound practice from novice to expert. The aim is to ensure Respiratory trainees achieve the primary operator level without the difficulties currently faced. The expectations for primary operator level 4 (independent practice) are highly achievable and the availability of local mentors within Respiratory Medicine should streamline the process.




Excellent summary Chris.
The BTS standards seem a little over the top and over complicated. In a world where Medstudents will have early and ongoing ultrasound exposure, this level of granularity really diminishes a physicians capability to be an adult learner.
Imagine if we wrote a similar framework for using a stethoscope…