A 35 year old lady, Ms H, with a background of intravenous drug use, presented at night to the Emergency Department (ED) of a District General Hospital with sepsis of unknown source. She was treated with broad spectrum antibiotics and intravenous fluids by the ED team and referred for medical admission.
On assessment by the medical team she was drowsy and febrile with a labile blood pressure. A pansystolic murmur was audible on auscultation.
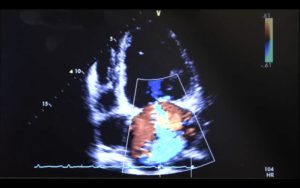
A bedside echocardiogram was performed in the ED by the medical SHO (FICE, CUSIC, RCEM L1 and Thoracic Level 1 accredited) due to the strong differential diagnosis of infective endocarditis. This revealed a large mitral valve vegetation with mitral regurgitation and a smaller aortic valve vegetation with severe aortic regurgitation. A CT head was performed revealing several small septic emboli.
PLAX showing large MV vegetation & AV vegetations.
Ms H required transfer to the regional cardiothoracic centre due to cardiovascular instability alongside severe valvular dysfunction after the cardiology team reviewed the bedside ultrasound images. The views acquired were of high quality and the cardiology team did not require further imaging prior to the transfer. She underwent a mitral valve & aortic valve replacement and required septal repair for where the mitral valve vegetation had eroded through the septal wall. She was discharged, cognitively intact, after completing a 6 week course of antibiotics tailored to blood culture positive Meticillin-Sensitive Staphylococcus aureus.
PLAX showing severe AR.
The use of bedside ultrasound in this case enabled diagnosis and accelerated the patient journey facilitating early transfer to a specialist centre. Without this frontline imaging Ms H may have waited several days for a formal departmental echocardiogram thus delaying life-saving interventions. It is feasible to consider that Ms H may not have survived the typical three-day wait for formal imaging. Incorporating these skills into specialist training can empower acute specialties and hasten diagnosis to improve the patient journey. Training and full-time accessibility to ultrasound is vital to ensure competence and enables high quality care and diagnosis at the frontline for our patients.
PSAX at level of MV.